The demand for integrated clinical software has never been higher. For maternal-fetal medicine (MFM) practices, these solutions aren’t just nice to have—they’re becoming essential. These tools help streamline workflows, enhance patient outcomes, and ultimately, raise the overall quality of care provided.
Why Integration Matters in Perinatal Care
Maternal-fetal medicine is a highly specialized field, that requires a lot of coordination between healthcare providers to ensure the best outcomes for both mom and baby. Traditional systems often involve tools that don’t communicate effectively, leading to fragmented care, inefficiencies, and even potential risks for patients. This is where integrated clinical perinatal software comes in. It offers a seamless connection between different parts of the healthcare ecosystem.
Integration matters because it synchronizes data across systems like electronic health records (EHR), ultrasound imaging, lab results, and more. When these systems communicate effectively, MFM practices can access comprehensive patient information in real-time, reducing the likelihood of errors and ensuring accurate care decisions based on the most up-to-date information.
How Integration Improves Workflow Efficiency and Accuracy
One of the most significant benefits of integrated clinical perinatal software is how it streamlines workflows. In a typical MFM practice, doctors, sonographers, nurses, and other providers must collaborate closely, but often have to juggle multiple platforms to access the information they need. This can be time-consuming and prone to mistakes.
With an integrated system, providers can work within a single, unified platform. For example, when an ultrasound is performed, the images and data are automatically uploaded to the patient’s EHR, allowing immediate access to all relevant information. This saves time and reduces the risk of errors associated with manual data entry and cross-referencing between different systems.
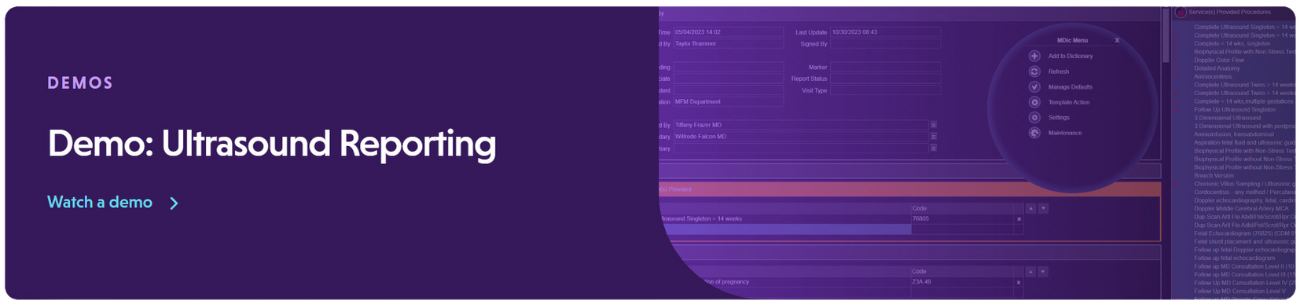
The Power of Integration in Ultrasound Reporting
Ultrasound reporting is a critical part of perinatal care, providing detailed visual and quantitative data that guide clinical decisions. In traditional systems, ultrasound data is managed in a separate system from the patient record, which can create bottlenecks in accessing this vital information. Integrated clinical perinatal software changes that by bringing ultrasound data directly into the main patient management system, offering several advantages:
- Automatic Data Transfer: Ultrasound images and measurements are automatically transferred into the patient’s electronic health record (EHR), eliminating manual uploads and reducing the risk of data loss or transfer errors.
- Real-Time Access: Providers can access ultrasound data right away, allowing for quicker diagnosis, which is particularly important in high-risk pregnancies where timely intervention can make a significant difference in outcomes.
- Enhanced Collaboration: Multiple Providers can view and discuss ultrasound findings simultaneously, regardless of their location, fostering better collaboration and more coordinated care.
- Faster Reporting: Automatically populate ultrasound reports using standardized templates, saving time and ensuring consistency and compliance with clinical guidelines.
- Improved Data Analytics: Combining ultrasound data with other patient information enables advanced analytics that can reveal trends in patient care, leading to better management of high-risk cases and improved outcomes.
Better Patient Outcomes Through Connected Care
Integrated clinical perinatal software doesn’t just help healthcare providers; it also has a positive impact on patient outcomes. With all relevant data at their fingertips, clinicians can make more informed decisions, leading to more personalized care.
For instance, if an ultrasound shows a potential issue, the integrated system can alert the clinician in real-time, allowing them to take action. This proactive approach is crucial in perinatal care, where early detection and intervention can make a big difference in the health of both mother and baby.
Also, integrated systems often include patient portals that allow expectant mothers to access their medical information, appointment schedules, and educational resources. This empowers patients to take an active role in their care and improves the patient-provider relationship.
The Growing Market for Clinical Perinatal Software
According to Global Market Insights, the clinical perinatal software market is expected to exceed $2 billion by 2032, driven by the increasing adoption of advanced technologies in maternal-fetal medicine. This growth is fueled by the number of pregnancy-related complications and the growing government initiatives and awareness regarding fetal care.
The report highlights that the demand for integrated solutions, especially those that incorporate ultrasound reporting, will continue to rise as healthcare providers look to improve clinical outcomes while reducing costs. For MFM practices, investing in integrated clinical perinatal software isn’t just about keeping up with trends—it’s about future-proofing their operations and delivering the highest standard of care.
Meeting the Demand
The rising demand for integrated clinical perinatal software is driven by the need for efficiency, accuracy, and improved outcomes in maternal-fetal medicine. Practices that adopt these integrated solutions will be better positioned to handle the challenges of modern perinatal care.
At AS Software, we understand the unique needs of MFM practices and have designed our solutions to support seamless integration across all areas of perinatal care, including advanced ultrasound reporting. For over three decades, we’ve been committed to providing our clients with the most advanced tools, enabling them to provide the highest quality of care.
As the demand for integrated clinical perinatal software continues to grow, it’s clear these solutions are the future of maternal-fetal medicine. Practices that embrace this technology will not only improve their operational efficiency but also enhance the quality of care they provide, leading to better outcomes for both mothers and babies.